Understanding Pregnancy Tests

Understanding Pregnancy Tests:
Your First Step Towards Motherhood and beyond.
In This Article:
-
Published
-
Last Modified
Tags
Discover the essentials of a pregnancy test, from how they work to the different types available and what steps to take after getting your results. This guide offers peace of mind as you embark on your journey to motherhood.
Pregnancy tests are the first beacon of information in your journey towards motherhood. They detect the presence of human chorionic gonadotropin (hCG), a hormone your body produces during pregnancy. Highly accurate, these tests offer reassurance and a preliminary confirmation of pregnancy, paving the way for the exciting journey ahead.
How does a Pregnancy Test Work?
Pregnancy tests search for hCG in your urine, which your body starts producing shortly after a fertilised egg attaches to your uterus. This hormone’s levels double every two to three days in early pregnancy, making urine and blood tests highly effective ways to confirm pregnancy. While home tests offer privacy and quick results, blood tests at your doctor’s office can confirm pregnancy earlier and more accurately.
Over-the-counter (OTC) tests detect the HCG hormone in urine, with various methods depending on the chosen kit. You might dip a stick into collected urine, use an eyedropper for transferring urine to a container, or place the stick directly in your urine stream mid-flow.
Home pregnancy tests boast a near-99% accuracy rate when used as directed by the Office on Women’s Health. These tests offer privacy, simplicity, and quick results, usually within minutes. Results could appear as a color change, a line, a symbol (like a plus or minus), or explicitly as “pregnant” or “not pregnant.” A negative outcome might not be definitive, especially if instructions weren’t followed, the test was taken too soon, or certain medications interfered. Consult a pharmacist about potential medication effects on test results.
If symptoms persist or your period doesn’t commence, try another test in a week. Seek GP advice for continuous negative results without menstruation. Some pharmacies and GPs provide tests, sometimes free or for a nominal fee, ensuring even quicker answers. Remember, if going to your GP, bring a urine sample in a clean container. Results can take days, though some tests are instant.
Wondering when to take a pregnancy test?
Some highly sensitive tests can detect pregnancy before your period is due. Yet, waiting until the first day of a missed period boosts accuracy. For the clearest result, test a week after missing your period.
Tests measure HCG, a hormone present only during pregnancy. This hormone appears after a fertilized egg attaches to the uterus, a process known as implantation, occurring about 10 days post-conception. HCG traces can appear 6 days post-implantation, but levels usually need 7–10 days to become detectable. If your cycles are irregular, testing 21 days after unprotected intercourse is wise. Testing too early may yield inaccurate results.
Types of Pregnancy Tests
Opt for Home Pregnancy Tests: Seeking a convenient option? Home pregnancy tests offer privacy. Conduct these tests as soon as you miss your period. They promise up to 99% accuracy when used as directed.
Consider Blood Tests: Need an early confirmation? Blood tests, performed in healthcare settings, can provide it. Although less commonly used, they’re highly accurate for early detection. At London Pregnancy Clinic we can perform these tests and one of our phlebotomists will assist you.
Signs you may be pregnant
Spotting early pregnancy signs is crucial. If you notice any unusual changes, consider a pregnancy test. Here’s a restructured and concise guide to understanding these signs.
Missed Period: A hallmark sign, missing your period suggests it’s time for a test. While a standard cycle lasts about 28 days, they can range from 24–38 days. If over a month has passed without your period, testing is wise. However, stress, medication, and changes in birth control can also affect your cycle. Early pregnancy might show light spotting as the egg implants, which differs from a regular period. Consult a doctor for any bleeding with a positive test.
Cramping: Similar to menstrual cramps, early pregnancy might bring discomfort. If your period doesn’t follow, testing is advisable.
Breast Changes: Pregnancy increases estrogen and progesterone levels, leading to tender, fuller breasts and darker veins. These symptoms can also precede a period, so they’re not definitive of pregnancy.
Feeling Different: Early signs include nausea, food aversions, fatigue, and frequent urination. Pay attention to your body; any distinct changes might indicate it’s time for a test.
Failed Birth Control: No method is 100% foolproof. Pills might fail, especially if not used perfectly, and condoms can break. Despite the effectiveness of long-term options like IUDs, pregnancy is still possible. If experiencing other pregnancy signs, take a test, regardless of your birth control use.
Remember, understanding your body’s signals is key. If you’re encountering any of these symptoms, a pregnancy test can provide early insight, allowing for prompt healthcare consultation. At London Pregnancy Clinic, we’re here to support you with tailored advice and comprehensive care for your pregnancy journey.
Embarking on Your Journey
A positive test marks the start of a remarkable journey. Your next move? Book an appointment with your healthcare provider. This crucial visit can verify your pregnancy with additional tests. It also kick-starts vital prenatal care, safeguarding your well-being and your baby’s health. Embrace this journey, prioritising health and care from the outset. Your provider will guide you through each step, ensuring you and your baby thrive.
At the LPC, we understand the emotional and physical significance of this phase in your life. Recognising the unique needs and concerns of expectant mothers, LPC offers the opportunity to book your first appointment directly with a midwife. This personal touch ensures that you receive tailored advice and support right from the outset.
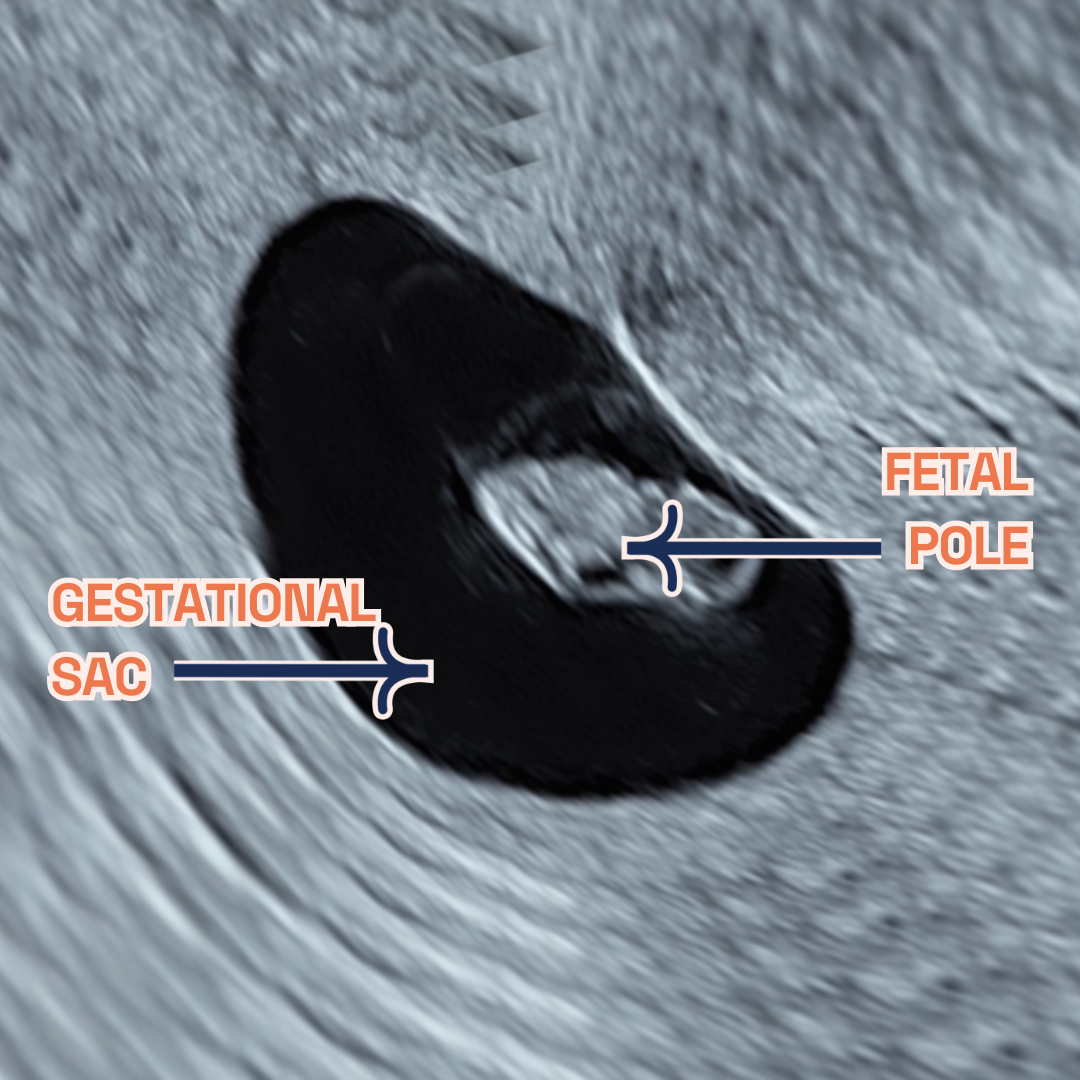
Furthermore, LPC introduces an option that diverges from the standard NHS protocol. Recognising the desire for early reassurance, we offer a viability scan as early as 6-9 weeks into the pregnancy. This service caters to those eager for an earlier confirmation of their pregnancy’s progression, rather than waiting until the NHS’s 12-week scan. The decision to opt for this early scan underscores the importance of peace of mind and the value of early connection with the developing life within.
The viability scan presents a window into the womb, offering expectant parents their first glimpse of their unborn child and the heartbeat that symbolises life. This experience often strengthens the bond between parent and child, grounding the reality of the pregnancy and fostering an early emotional connection.
Ultrasound Screening Vital for Early Detection
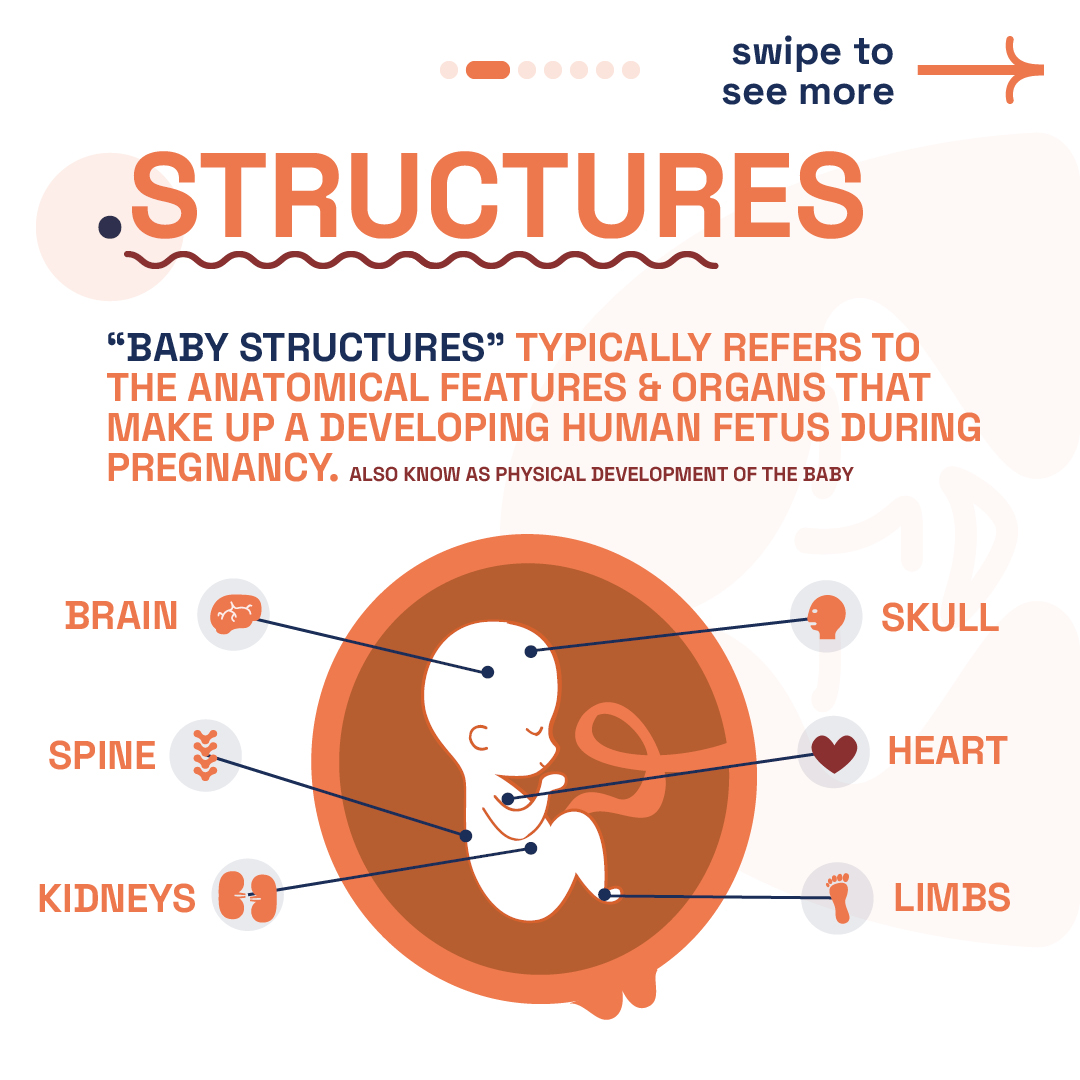
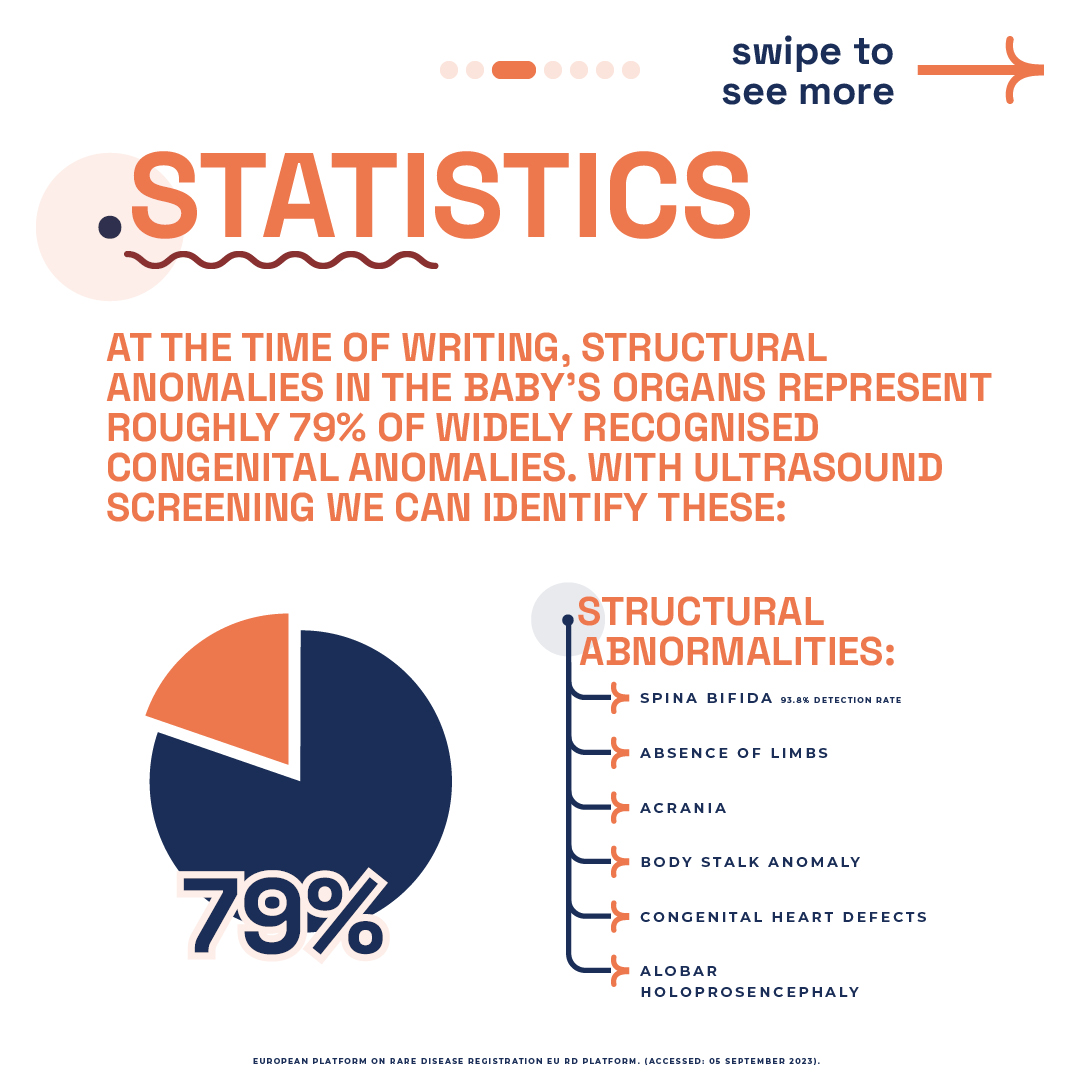
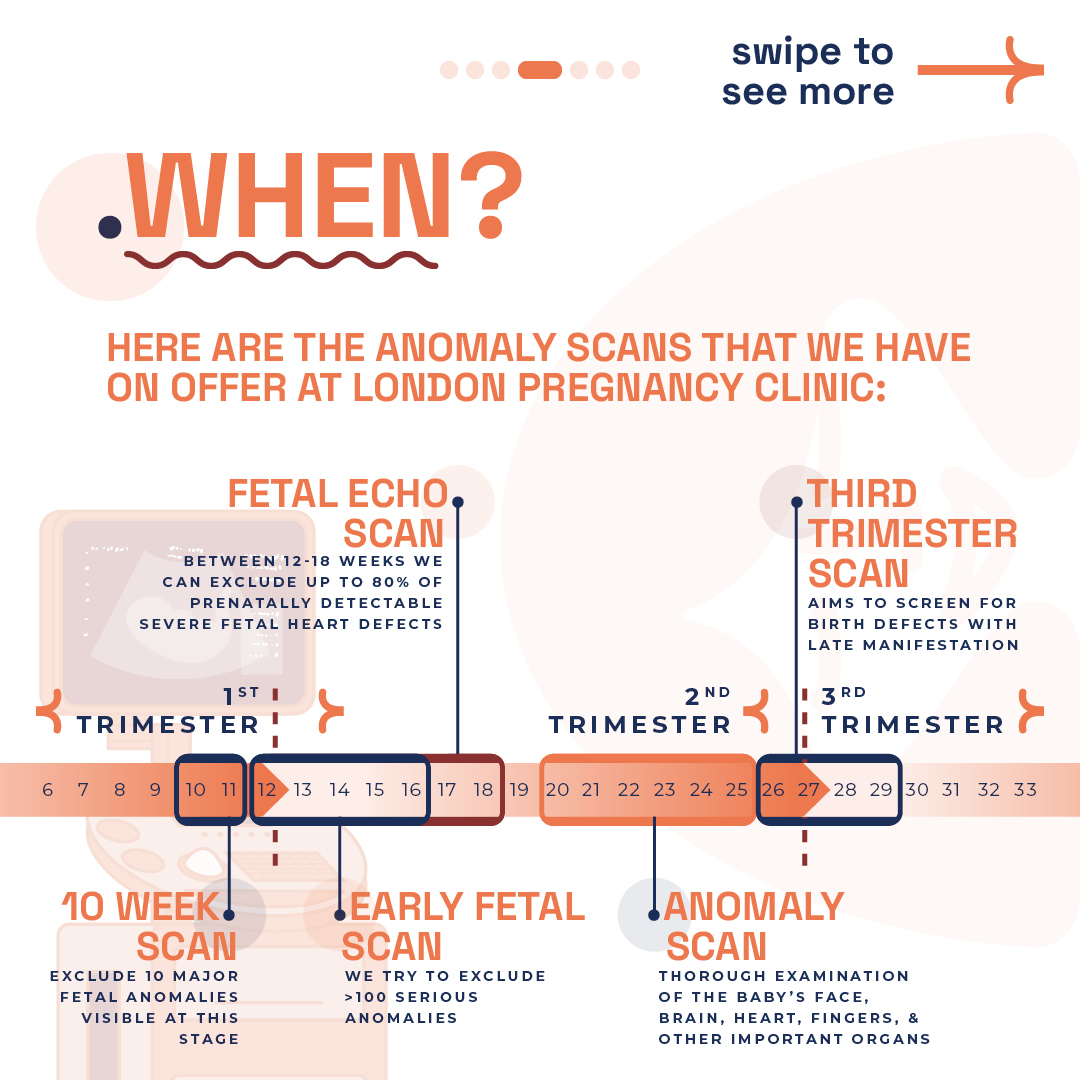
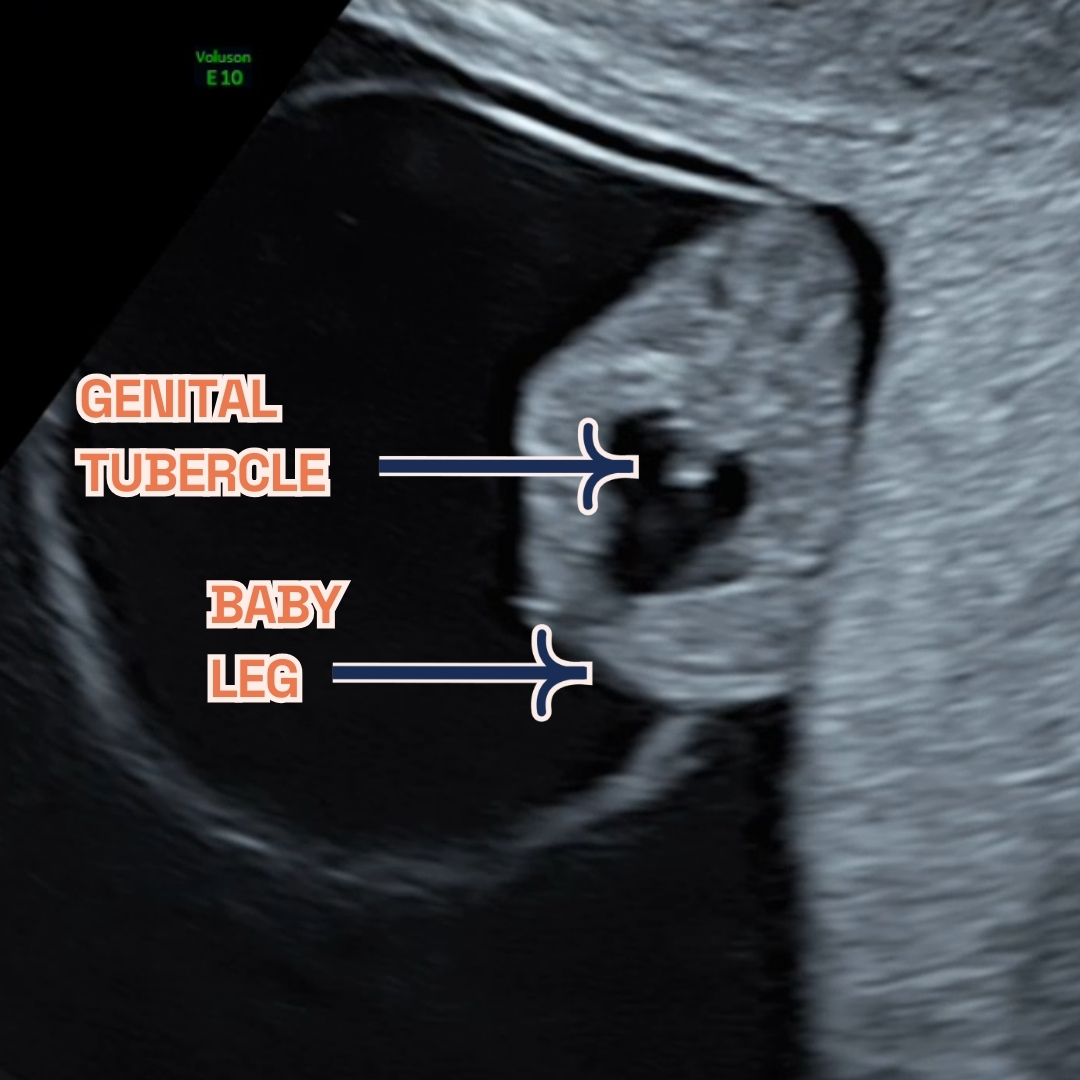
Ultrasound screenings are not just routine checks; they’re crucial for early prenatal care. These scans help identify potential structural anomalies in the baby’s development, which are pivotal for addressing congenital anomalies. At London Pregnancy Clinic, we specialise in providing comprehensive ultrasound screenings, tailored to each stage of pregnancy, ensuring early detection and peace of mind from 10 weeks onward.
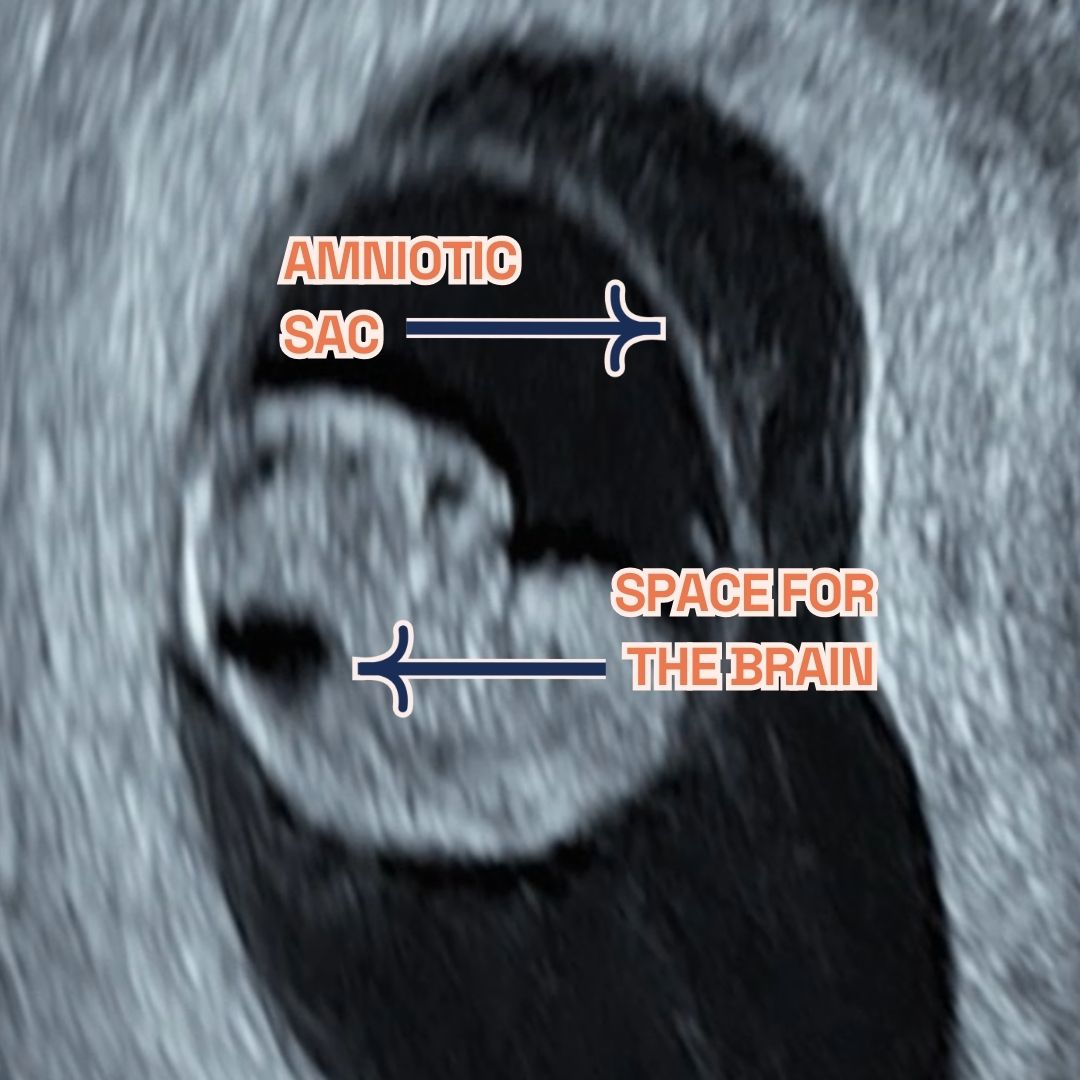
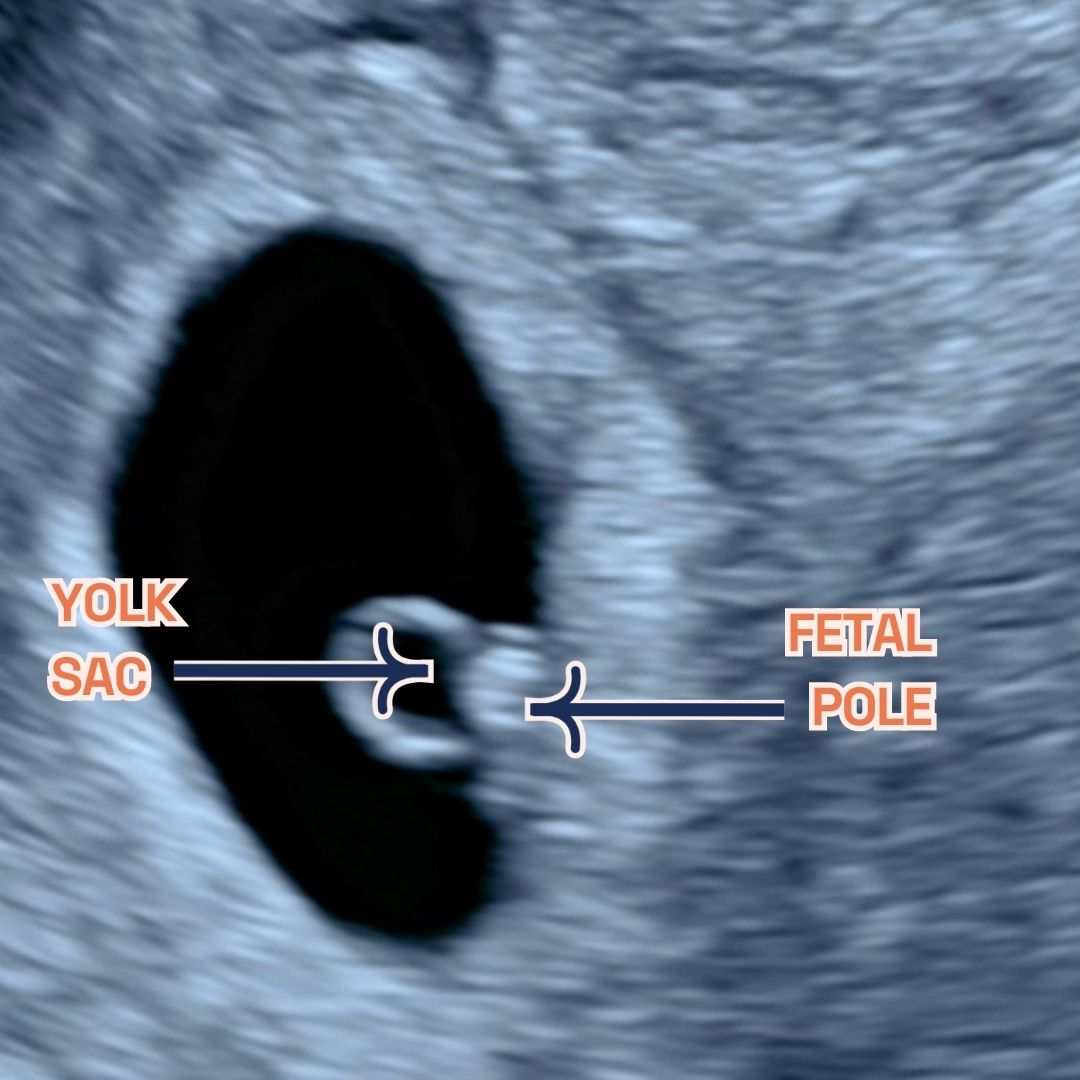
Many inquire about the possibility of conducting a scan at 4 weeks. However, at such an early stage, the ultrasound reveals limited details, often not enough to confirm a pregnancy. By 5 weeks, while we may observe the gestational and yolk sacs, these findings alone do not confirm pregnancy viability. It’s this understanding that shapes our recommendation for the optimal timing of your first scan to be held off until week 6/7.
Our 10 Week Scan stands out, offering a unique glimpse into the womb to detect 10 critical fetal anomalies. This pioneering scan, exclusive to our clinic, aligns perfectly with Non-Invasive Prenatal Testing (NIPT), elevating the standard of prenatal care available to you.
The cornerstone of our scanning services, the Early Fetal Scan, provides an in-depth examination aimed at identifying over 100 serious anomalies well before the standard NHS 19-20 week scan. This early insight grants expectant parents the reassurance and crucial information needed during these formative weeks.
Our approach to prenatal screenings is revolutionary, offering early answers and invaluable peace of mind. Through our advanced screening capabilities, we illuminate potential concerns, facilitating timely interventions. These scans are more than mere procedures; they are essential milestones providing reassurance that your baby’s development is on course, empowering you to manage your pregnancy with informed confidence and proactive care.
Final Thoughts
At the London Pregnancy Clinic, we’re here to support you from the very first step. If you’ve taken a pregnancy test and are ready for the next stage, or if you have questions about pregnancy tests, our team is here to assist you. You can use our EDD calculator to figure out when your baby might arrive.