Hertility x LPC partnership

Hertility x LPC partnership:
Bringing Fertility and pregnancy ultrasound support for women
-
Published
-
Last Modified
Tags
Discover the transformative partnership between Hertility and London Pregnancy Clinic, revolutionising the way you access fertility and pregnancy ultrasound services. From early pregnancy to specialised scans, our collaboration ensures you receive world-class care without the wait, at a price you can afford.
In an exciting development for expectant mothers and those on their fertility journey, Hertility has partnered with us, London Pregnancy Clinic (LPC), transforming access to reproductive healthcare. Understanding the emotional toll of waiting for your first pregnancy scan, we’ve come together to offer you world-class scanning facilities, ensuring early reassurance through ultrasound without the long wait. It promises to bridge the gap between fertility understanding and pregnancy care, offering an integrated approach to women’s health that is both convenient and comprehensive. Both fertility and pregnancy ultrasound are very important and we are going to unpack what we can offer.
Who is Hertility?
In 2020, Hertility was conceived with a distinct vision by Dr. Helen O’Neill, Dr. Natalie Getreu, and Deirdre O’Neill. It sprang from a realisation that women’s health complexities were often overlooked, with conditions remaining enigmatic within the healthcare system. Hertility emerged as a beacon, championing the cause of bringing reproductive science into the hands of women globally.
Tired of the gaps in women’s healthcare, Hertility was born out of necessity. It became clear that the data underpinning women’s health was not only insufficient but also largely based on male physiology, leading to a paradigm shift in approach. Dr. O’Neill, through her fifteen years in academia, recognised the urgency for tailored datasets that reflect the true nature of female health concerns. Hertility is not just a company; it’s a movement towards empowering women with the knowledge to make informed decisions about their health and life choices.
Why was Hertility Created?
The inception of Hertility was motivated by the profound desire to address the elephant in the womb – the inherent complexities of female reproductive health. With a staggering 60% of women grappling with hormone and gynae issues and the diagnosis of fertility disorders stretching up to eight years, Hertility’s founders saw the dire need for change. By empowering women with accessible, research-led health assessments, Hertility is breaking barriers and shining a light on the path to understanding and managing women’s health effectively.
Hertility’s resolve to be research-led has set a new standard in women’s healthcare. It stands firmly on the foundation of clinical trials and extensive data collection, ensuring every insight provided is robust and actionable. Hertility’s comprehensive at-home hormone and fertility tests are more than just diagnostics; they are a clarion call to acknowledge and act on women’s reproductive health needs. The company’s commitment to sharing their findings reflects their ethos of transparency and education, making Hertility a true vanguard in the realm of women’s health.
Why Hertility and LPC?
Hertility is at the forefront of women’s health, offering at-home hormone and fertility test kits designed to empower women with knowledge about their reproductive health. Their comprehensive approach evaluates various factors, including hormonal balance, ovarian reserve, and potential reproductive health conditions, to provide actionable insights.
Understanding the importance of seamless care, Hertility’s partnership with LPC is a natural progression. LPC’s reputation for excellence in fertility and pregnancy ultrasound complements Hertility’s mission, providing a continuum of care that supports women from fertility assessment through to pregnancy. From fertility screening to anomaly scan we provide a large variety of services for women from our London clinic.
-

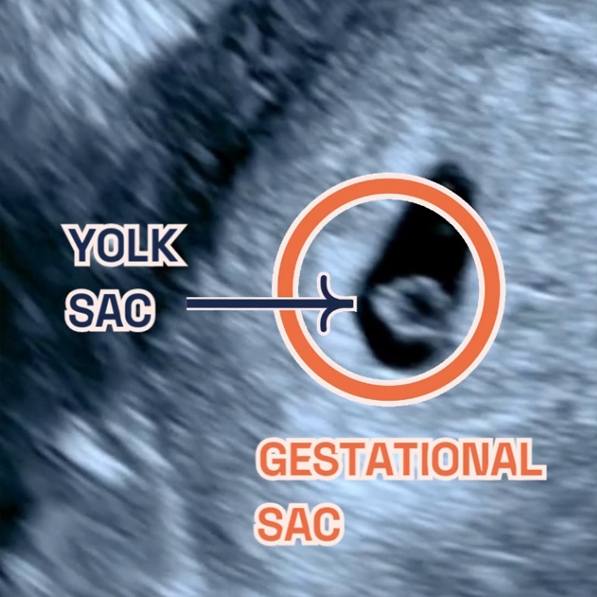
Viability scan 3D image
-
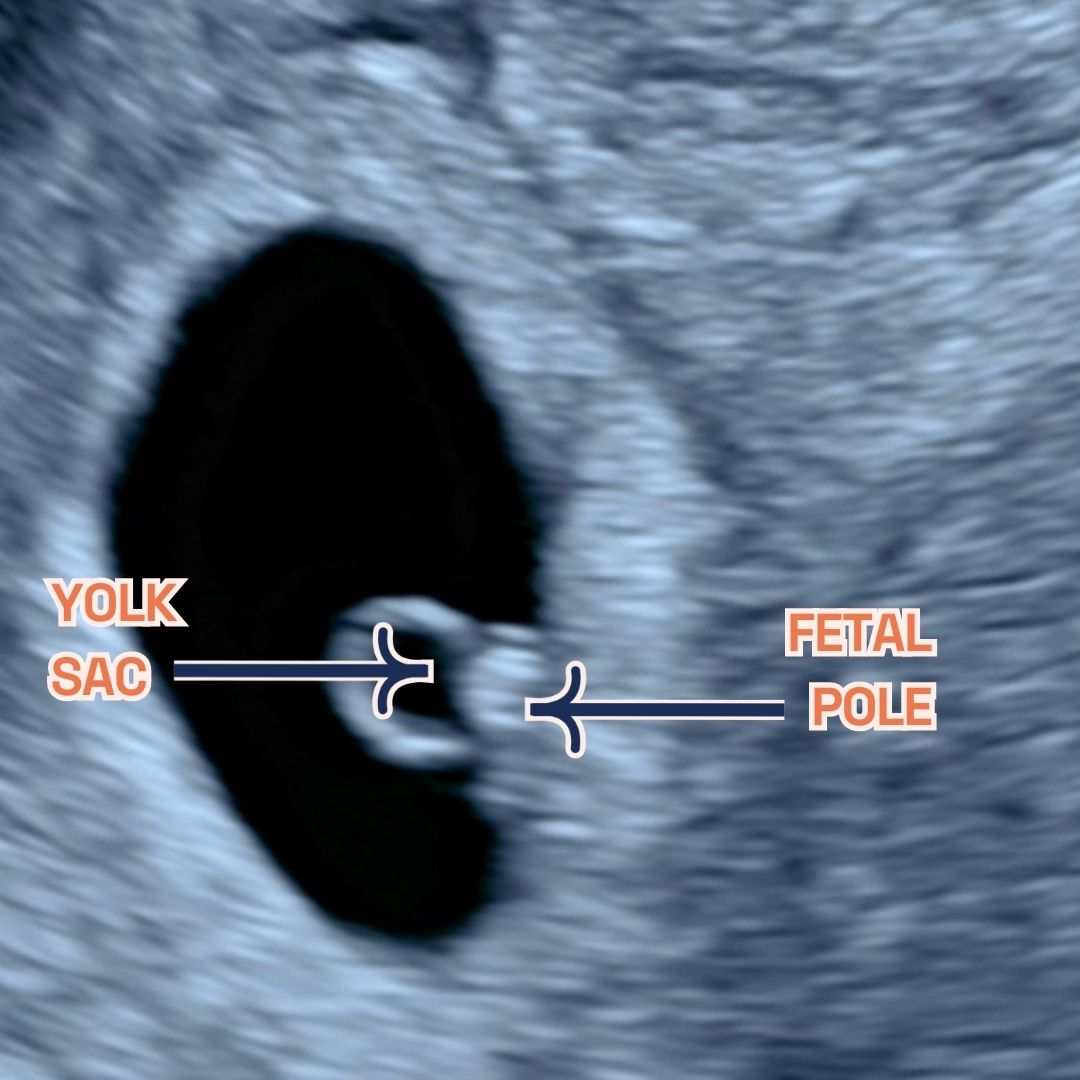
You can see the fetal pole, gestational sac and yolk sac at week 6.
Fertility and pregnancy ultrasound
- Early Pregnancy Scans: Available from 6 weeks, these scans offer early reassurance, confirming the presence of a gestational sac and fetal heartbeat. The first scan we offer is called the viability scan (or the 6-week scan).
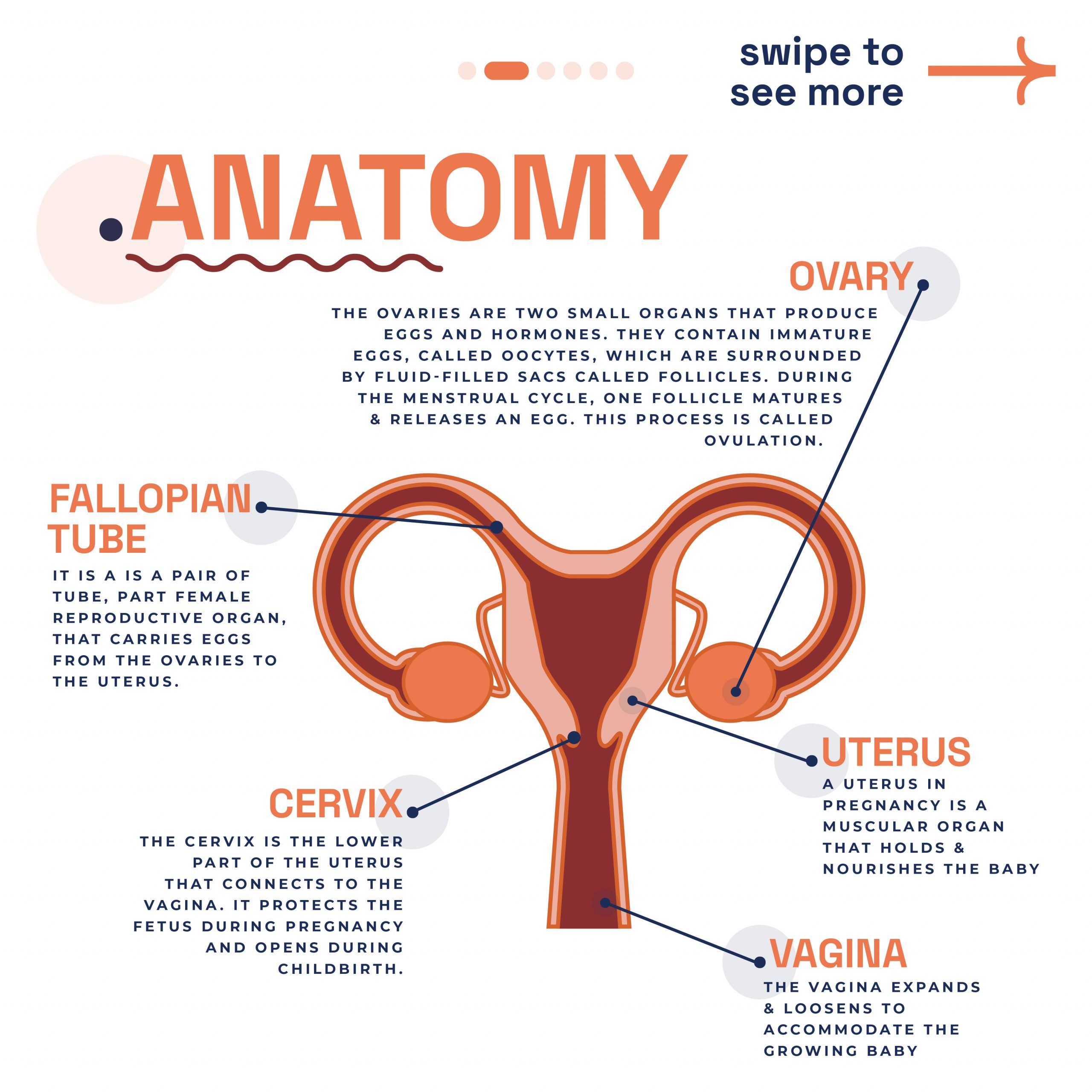
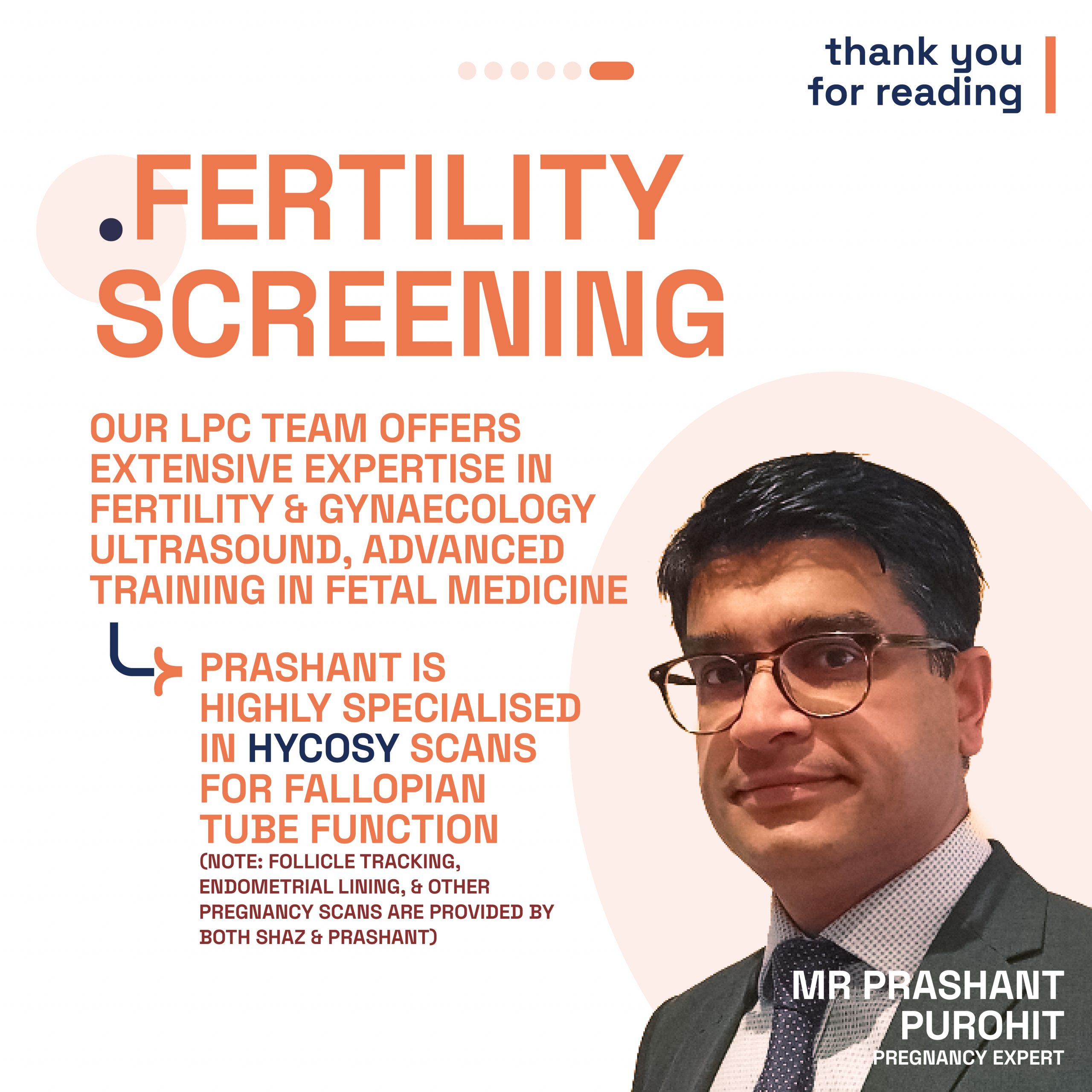
- HyCoSy Scans: For those investigating fertility concerns, HyCoSy scans assess tubal patency, crucial for understanding potential fertility issues.
- General, Anomaly, and Early Fetal Scans: A comprehensive range of scans ensures that every aspect of your pregnancy is monitored, from general health checks to detailed anomaly scans. We specialise in NIPT and 10 Week Scan, which is our signature early pregnancy scan.
All scans at LPC are conducted by consultant-level doctors or specialist sonographers in fetal medicine, gynaecology, and fertility. Overseen by Dr Fred Ushakov, a renowned specialist in fetal medicine and obstetrical ultrasound, our team guarantees the highest standard of care.
Why Wait? Early Scans Available from 6 Weeks
The first few weeks of pregnancy are a profound journey filled with anticipation and, sometimes, anxiety. Traditionally, expecting mothers wait until the 11 to 14-week mark for their first scan, a period filled with unanswered questions and needless worries. Recognising the importance of early reassurance, LPC opens its doors to Hertility customers for pregnancy scans starting as early as 6 weeks. Our goal? To provide you with the peace of mind that comes from knowing your pregnancy is progressing as expected, as soon as possible.
If you’re navigating the journey of fertility and pregnancy, let Hertility and LPC guide you to a path of informed, supported, and comprehensive care. You can check out our fertility and pregnancy ultrasound services!
Final thoughts
Hertility’s partnership with the London Pregnancy Clinic marks a defining moment in women’s health. With Hertility’s research-driven methodology and our fertility and pregnancy ultrasound services, we hope to provide a holistic approach for all women. Our combined effort provides an answer to the calls for early and accessible pregnancy scans, ensuring that expectant mothers receive the support and assurance they need, precisely when they need it. This collaboration goes beyond convenience; it is a powerful statement that women’s health deserves prioritisation and respect.